Beneath the Skin: The Problems Chronic Stress Can Cause

By: Editorial Staff
Categories:
Beneath the Skin: The Problems Chronic Stress Can Cause
From occupational stress to mental illness.
Posted December 11, 2021 | By: Odessa S. Hamilton MSc, MBPsS, FRSPH
KEY POINTS
- The Sars-CoV-2 outbreak caused a proliferation in occupational demands that has become an increasingly more salient threat to our mental health.
- Stigmatization and fear of penalization reduces health-seeking behaviors and workplace transparency of mental distress.
- Being in a chronic state of stress at work can disrupt the body’s dynamic physiological balance, resulting in psychopathological conditions.
- Stress-induced mental illness comes at a colossal annual cost to global economies, so whether felt or seen, we all pay a price.
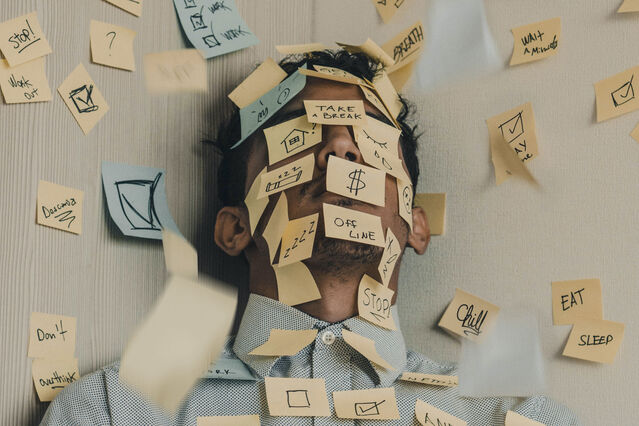
Source: Featured Image by Luis Villasmil | Unsplash
Non-existent work-life balance. Difficult boss. Dysfunctional team. Impossible workload. Transit traumas. Toxic company culture. Dangerous conditions. Precarious schedules. Underemployed. Undervalued. Underpaid.
Most of us have experienced one or more of these occupational stressors to varying degrees, but few understand what it truly costs us and how it affects our biology. Through an interdisciplinary lens, let us delve beneath the skin to understand why reducing these daily work-related burdens is critical to our health and economy. While work has historically consumed a significant proportion of our daily lives, the recent proliferation of occupational demands has become an increasingly more salient threat to our mental health and immune responses.
Mental Fragility
Mental health is so very fragile. Anyone anywhere can lose it. Prior to the COVID-19 pandemic more than 1 billion people, 16 percent of the world’s population, reported experiences of mental illness, accounting for 7 percent of the global burden of disease (Rehm & Shield, 2019). Since the pandemic, mental health sequelae has become a distinct public health concern (Hamilton et al., 2021). Despite its pervasive nature, remarkably, mental illness remains taboo and continues to be underreported. It comes as no surprise then that the true incidence is unknown and what we see is likely the tip of the iceberg. The stigmatization and fear of penalization reduce workplace transparency and health-seeking behaviours (Bharadwaj et al., 2017). It contributes to why occupational stress remains a widely neglected influencer of mental distress.
Stress Awareness
Occupational stress is characterized as our appraisal of situational factors at work exceeding our individual resources, such that our psychobiological integrity is endangered (Lazarus & Folkman, 1984), a fancy way to explain when we feel overloaded, overburdened, and overwhelmed by work-related issues. It is well-documented and widely known that occupational stress can lead to mental ill-health, but how it occurs is less understood. Having an awareness of the process, even in its most basic form, can reveal the gravity of stress exposure at work. The hope is that it will lead us to approach it with the solemnity it deserves.
The Physiological Response
Occupational stress is implicated in a dysregulated immune response (Toker et al., 2005). In line with this, advances in molecular medicine have shown that inflammation is a principal component in the onset and progression of disease (Moutsopoulos & Madianos, 2006). Good stress (in the vernacular) is processed adaptively and there are benefits to transient inflammatory responses. However, acute, or prolonged work-stress exposure can impair anti-inflammatory effects on immunity, while inhibiting the interplay between immune cells and signaling networks (Bae et al., 2019). This leads to alterations of immune function at tissue and cellular levels (Kiecolt-Glaser et al., 2002).
Delving Deeper
As part of the protective action of the stress response, a range of neurotransmitters, hormones, and acute-phase reactants mediate allostasis (the constant, dynamic bodily response to maintain physiological stability; McEwen, 2002). This inflammatory cascade is designed to eliminate microbial pathogens, induce tissue repair, and restore homeostasis (Rohleder, 2019). However, when the body is repetitively challenged, such as in the case of daily occupational stressors, allostatic systems are overstimulated, which develops a cumulative biological burden (wear and tear) on the body and brain, called allostatic load (Sun et al., 2007). Allostatic load presents in a variety of negative forms, including hippocampal atrophy, with the hippocampus brain structure being a site of structural and functional pathology that is involved in most mental health conditions (McEwen, 2007). Therefore, being in a chronic state of stress at work can disrupt the body’s dynamic physiological balance, resulting in conditions of poor mental health (Priyadarshini & Aich, 2012).
All the ‘Ologies
Stress (psychology) activates the network between the brain (neurology), the endocrine system (endocrinology), and the immune system (immunology) in the provocation of an inflammatory response that results in mental ill-states. Psycho-neuro-immunology has been identified as a plausible, causal framework through which this integrative interaction occurs (Ader & Cohen, 1975). The interplay between this network is dependent upon feedback-loops interacting to maintain homeostatic and allostatic equilibrium (Lorentz, 2006). When this interaction is working well it is adaptive, but when it is disrupted or overstimulated by stress, it leads to biological dysfunction and poor mental health outcomes.
The Economics of Breaking Minds
Within major global economies, occupational stress has risen to six in 10 employees (GOS, 2021). China reports the highest global incidence of workplace stress at 86 percent (GOS, 2021), with the U.S. and U.K. trailing marginally behind at 75 percent (APA, 2021; MHF, 2018). This comes at a colossal annual cost to global economies, an estimated $300 billion in the U.S., £28.3 billion in the U.K., and $14 billion in Australia (Boyd, 2021; GOS, 2021). Nonstop work cultures are clearly a false economy. Whether seen or unseen, we all pay a price. Still, we see these figures, ignore these figures, then proceed to proverbially work ourselves into the ground. We continue to operate within high-load, high-stress environments, under the guise of productivity gains and economic advantage—desperately hopeful that the mind won’t break.
Cut the Stigma
Stress reductions are expected to improve mental health, prevent disease, reduce organizational waste, and curtail public spending (Wright et al., 2020). Rethink stress and how it relates to mental illness. Remove mental health issues from the periphery. Have honest conversations with managers, colleagues, friends, and family. Be transparent about moments of mental distress, cut the stigma.
Prevention is Better Than Cure
Sawhney et al. (2018) proposed seven stress recovery strategies: work-related talks, stress-related talks, personal time, exercise, recreational activities, relaxation, and having mastery experiences. Ultimately, mental health needs to become a regular discussion that can be shared without judgment or penalty, because no person is immune to it. Work should be a safe place that promotes health from a broad perspective, because there is no health without mental health.
References
Ader, R., & Cohen, N. (1975). Behaviorally Conditioned Immunosuppression: Psychosomatic Medicine, 37(4), 333–340. https://doi.org/10.1097/00006842-197507000-00007
APA, American Psychological Association (2019). Stress. https://www.apa.org. https://www.apa.org/topics/stress/index
Bae, Y.-S., Shin, E.-C., Bae, Y.-S., & Van Eden, W. (2019). Editorial: Stress and Immunity. Frontiers in Immunology, 10. https://doi.org/10.3389/fimmu.2019.00245
Bharadwaj, P., Pai, M. M., & Suziedelyte, A. (2017). Mental health stigma. Economics Letters, 159, 57–60. https://doi.org/10.1016/j.econlet.2017.06.028
Boyd, D. (2021). Workplace Stress. The American Institute of Stress. https://www.stress.org/workplace-stress
GOS, Global Organisation for Stress (2021). STRESS FACTS | Global Organization for Stress. http://www.gostress.com/stress-facts/
Hamilton, O. S., Cadar, D., & Steptoe, A. (2021). Systemic inflammation and emotional responses during the COVID-19 pandemic. Translational Psychiatry, 11(1), 1–7. https://doi.org/10.1038/s41398-021-01753-5
Kiecolt-Glaser, J. K., McGuire, L., Robles, T. F., & Glaser, R. (2002). Psychoneuroimmunology: Psychological influences on immune function and health. Journal of Consulting and Clinical Psychology, 70(3), 537–547. https://doi.org/10.1037/0022-006X.70.3.537
Larson, S. J. (2002). Behavioral and Motivational Effects of Immune-System Activation. The Journal of General Psychology, 129(4), 401–414. https://doi.org/10.1080/00221300209602104
Lazarus, R. S., & Folkman, S. (1984). Stress, Appraisal, and Coping. Springer Publishing Company.
Lorentz, M. (2006). Stress and Psychoneuroimmunology: 11, 11.
McEwen, B. S. (2002). Sex, stress and the hippocampus: Allostasis, allostatic load and the aging process. Neurobiology of Aging,23(5), 921–939. https://doi.org/10.1016/S0197-4580(02)00027-1
McEwen, B. S. (2007). Physiology and Neurobiology of Stress and Adaptation: Central Role of the Brain. Physiological Reviews,87(3), 873–904. https://doi.org/10.1152/physrev.00041.2006
MHF, Mental Health Foundation (2018, May 14). Stress: Are we coping? Mental Health Foundation. https://www.mentalhealth.org.uk/publications/stress-are-we-coping
Moutsopoulos, N. M., & Madianos, P. N. (2006). Low-Grade Inflammation in Chronic Infectious Diseases: Paradigm of Periodontal Infections. Annals of the New York Academy of Sciences, 1088(1), 251–264. https://doi.org/10.1196/annals.1366.032
Priyadarshini, S., & Aich, P. (2012). Effects of Psychological Stress on Innate Immunity and Metabolism in Humans: A Systematic Analysis. PLOS ONE, 7(9), e43232. https://doi.org/10.1371/journal.pone.0043232
Rehm, J., & Shield, K. D. (2019). Global Burden of Disease and the Impact of Mental and Addictive Disorders. Current Psychiatry Reports, 21(2), 1–7. https://doi.org/10.1007/s11920-019-0997-0
Rohleder, N. (2019). Stress and inflammation – The need to address the gap in the transition between acute and chronic stress effects. Psychoneuroendocrinology, 105, 164–171. https://doi.org/10.1016/j.psyneuen.2019.02.021
Sawhney, G., Jennings, K., Britt, T., & Sliter, M. (2018). Occupational Stress and Mental Health Symptoms: Examining the Moderating Effect of Work Recovery Strategies in Firefighters. Journal of Occupational Health Psychology, 23(3), 443–456. https://doi.org/10.1037/ocp0000091
Sun, J., Wang, S., Zhang, J.-Q., & Li, W. (2007). Assessing the cumulative effects of stress: The association between job stress and allostatic load in a large sample of Chinese employees. Work & Stress, 21(4), 333–347. https://doi.org/10.1080/02678370701742748
Toker, S., Shirom, A., Shapira, I., Berliner, S., & Melamed, S. (2005). The Association Between Burnout, Depression, Anxiety, and Inflammation Biomarkers: C-Reactive Protein and Fibrinogen in Men and Women. Journal of Occupational Health Psychology, 10(4), 344–362. https://doi.org/10.1037/1076-8998.10.4.344
Wright, B. J., Eddy, P. J., & Kent, S. (2020). Work Stress, Immune, and Inflammatory Markers. In T. Theorell (Ed.), Handbook of Socioeconomic Determinants of Occupational Health: From Macro-level to Micro-level Evidence (pp. 1–19). Springer International Publishing. https://doi.org/10.1007/978-3-030-05031-3_28-1
